December 27, 2025
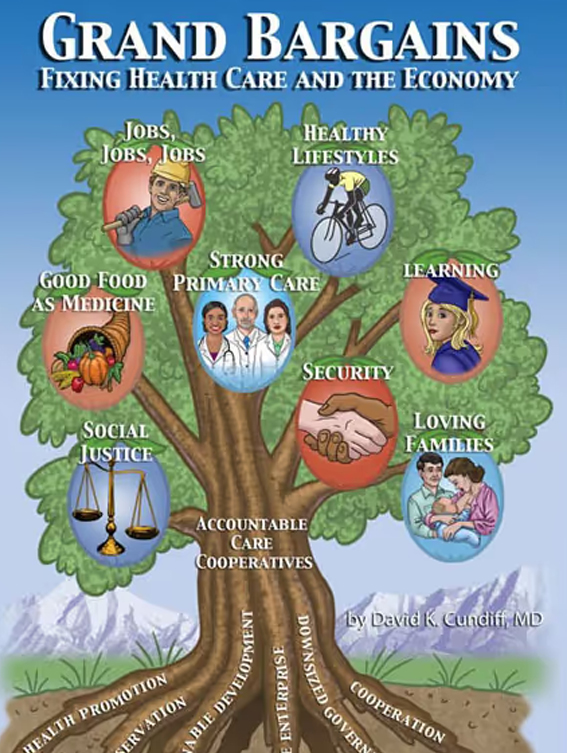
Accountable Care Cooperatives offer a bipartisan, community-owned solution to the healthcare crisis. Explore how this 'Grand Bargain' can fix a broken system.
Accountable Care Cooperatives (ACCs): A Community-Owned Healthcare Fix
After the longest government shutdown in U.S.history—triggered by battles over healthcare funding—the core issue remainsunresolved. Neither political party has produced a durable solution. TheCenters for Medicare and Medicaid Services (CMS) projects U.S.healthcare spending will reach nearly $9 trillion by 2035, consuming 20% to 22%of our GDP.
Without significant policy changes, the CongressionalBudget Office projects healthcare spending will hit 31%of GDP by 2035 and a staggering 46% by 2080. The consequences aredire: soaring premiums, faster Medicare insolvency, suppressed wage growth, anddiminished global competitiveness; and the continuedshift toward high-deductible plans. Demographic pressures—including rapidMedicare enrollment by the baby-boom generation—and high-cost drugs such asGLP-1s and gene therapies further accelerate spending. The media constantlyreports on the effect of the health care funding crisis on everyday Americans,facing higher premiums or losing health care insurance altogether.
As former White House Chief of Staff Rahm Emanuel suggests,moments of crisis open the space for ideas that once seemed impossible.
Accountable Care Cooperatives (ACCs) propose a transformative, community-owned model that restructures the U.S. health system from the ground up. These private, nonprofit, member-owned organizations unify medical care with housing, nutrition, mental health, and other social supports through a single local structure. Rooted in self-reliance, cooperation, and democratic governance, ACCs aim to solve both the healthcare and economic crises.
Consequencesinclude soaring insurance premiums and out-of-pocket costs; rising Affordable Care Act premiums; reduced federal investment in education, infra structure, research, and defense; faster Medicare insolvency; suppressed wage growth;diminished global competitiveness; and the continued shift towardhigh-deductible plans. Demographic pressures—including rapid Medicareenrollment by the baby-boom generation—and high-cost drugs such as GLP-1s and gene therapies further accelerate spending.
Yet, as former White House Chief of Staff Rahm Emanuel suggests, moments of crisis also open political and civic space for ideas that once seemed impossible.
Unlike top-down federal mandates, ACCs are bottom-up, locally governed, innovative and completely transparent on four core metrics:
1. Quality of care
2. Cost of care
3. Health outcomes
4. Member satisfaction
Purpose and Urgency
This proposal leverages today’s healthfinancing crisis to advance a durable, bipartisan reform. It argues thata national ACC system can be implemented swiftly through federal legislation—ifsupported by informed civic engagement.
Transforming our fragmented system into one composedexclusively of ACCs would improve care quality while sharply reducing costs. TheCongressional Budget Office issued a long-term estimate of about $44 trillion as the GDP in 2035. Under anACC-based system, total healthcare spending would remain at $6.3 trillion peryear through 2035, falling to about 14.3% of GDP. This represents a dramaticimprovement over current projections.
Key Features of the ACC Model
- Integration of Health & Social Services: ACCs unify medical care with housing, nutrition, and mental health. A patient with diabetes might receive medical treatment alongside nutritional counseling and job placement—all within the same cooperative.
- Direct Primary Care (DPC): ACCs are anchored by DPC providers with smaller patient panels (750 patients vs. the current 2,500). Each ACC would be anchored by Direct Primary Care physicians, nurse practitioners, and physicians’ assistants, serving as patient-centered medical homes. With smaller patient panels (about 750 patients per provider instead of 2000 to 2500 patients), Direct Primary Care Primary Care Providers (PCPs) could devote more time to each individual, fostering trust, improving continuity, and enhancing satisfaction. Preventive and coordinated care reduce downstream costs while strengthening doctor–patient relationships. Research suggests that reducing patient panels allows for more personalized care, improved patient outcomes, and greater physician satisfaction.
- Self-Regulation and Flexibility: Instead of one-size-fits-all federal medical treatment rules, each ACC defines its own clinical guidelines, benefit packages, and priorities. Cooperatives would provide optional home-birth services and alternative therapies as well as telemedicine, chronic care, and rural outreach. Local control fosters responsiveness and innovation.
4. Global Budgets: Operatingunder capitated global budgets, ACCs would receive a fixed per-memberamount to cover all health and social services. This eliminates incentives forunnecessary tests or procedures and drastically reduces bureaucratic overhead.Savings are reinvested into expanded services, lower premiums, and communitydevelopment initiatives. With a minimum number of “covered lives” in an ACCbeing at least 1,000,000 people, ACCs would be very likely to stay viablefinancially overtime.
- Transparent Competition: People choose their ACC based on services, health outcomes, member satisfaction, and cost. Transparency is central: ACCs publicly report expenditures, health outcomes, and member satisfaction to foster trust and informed choice.
- Participatory Governance: Decision-making resides with members, staff, an elected board, and a CEO, who collaboratively set priorities and allocate resources. This builds legitimacy and ensures that services reflect any community’s unique demographic and cultural profile.
- Doubling Provider Trainees: To support manageable caseloads, enrollment in U.S. medical schools must at least double. To provide primary care physicians, nurse practitioners, and physician assistants with manageable caseloads (750 patients per primary care provider (PCP) instead of 2000-2500 per PCP) and to account for the increased number of seniors with more healthcare needs, enrollment in US medical schools must at least double.
Funding and Financial Structure
ACCs would befinanced through a diversified mix:
- Risk-Adjusted Block Grants: from the US Department of Health and Human Services (e.g., Areas with higher need receive more funding.)
- Member Premiums, locally adjusted by age, income, and demographics.
- Community and Philanthropic Investment: for innovation, experimentation, and infrastructure.
Strategies tofree resources for patient care, social services, and lower member premiums oreliminate out of pocket costs include stopping:
- Excessive Administration: Accounting for at least 30% of total healthcare costs, including public and private insurance-related expenses and administrative burden on healthcare providers.
- Unnecessary or harmful medical interventions: See my book, Money Driven Medicine—Tests and Treatments That Don’t Work.
- Fraud: Estimated to range from 3% to 10% of total healthcare spending by the National Health Care Anti-Fraud Association.
ACCs address thefull continuum of need:
1. UniversalCoverage: Every US resident is enrolled in an ACC, closing all gaps.
2. MedicalCare: Preventive care(screenings, vaccinations), chronic disease management, dental care, and mentalhealth/addiction services.
3. Long-TermCare: Home-based andassisted-living support—services often excluded from Medicare and privateplans.
4. SocialServices: Housingassistance, food security, job training, and financial counseling.
5. AlternativeTherapies: E.g.,acupuncture, massage, prolotherapy, and midwife-assisted births. CostSavings: Capitated funding rewards prevention and efficiency.
6. ImprovedHealth Outcomes: Coordinated,community-based care reduces chronic disease by addressing root causes.
7. EmpoweredCommunities: Local healthcareand social services governance strengthen civic trust, participation, andresilience.
The ACCframework aligns with the Grand Bargains financial strategy: freeze total government health funding at the 2026 level through 2035 while expandinguniversal coverage and decentralizing delivery (approx.$6.3 trillion in 2026 and annually projected to 2035, a huge jump from $5.6trillion in 2025).
The most cited and realistic estimates project that the cost of healthcare in the U.S. will be around $9trillion in 2035, consuming approximately 20% to 22% of thecountry's total economic output (GDP).
The Projected 10-Year Impact:
- $5 trillion saved on healthcare spending
- 23% reduction in the projected federal deficit
Five-Pronged Waste-Reduction Strategy
- Decentralize Regulation: Allow ACCs to develop their own clinical policies (e.g., choosing between bypass surgery or the Dr. Dean Ornish program for heart disease).
- Preserve Choice: Ensure patients and providers can choose their ACC.
- Mandate transparency—online disclosure of benefits, long-term care, and metabolic health programs (i.e., addressing obesity, type 2 diabetes, high blood pressure, and cardiovascular risks).
- Foster Competition: Compete on price, quality, and satisfaction.
- Freeze Spending: Cap government healthcare spending at 2026 levels through 2035.
Conclusion
Accountable Care Cooperatives represent a bold reimaginingof American healthcare—integrating universal access with fiscal responsibility.They advance the mission of the Grand Bargains project: rebuilding a societygrounded in solidarity, sustainability, and shared prosperity.
Call to Action
Pleaseforward this proposal to friends, family, and legislators. Questions orcomments? Email me at: grandbargainsbook@gmail.com
00). Each ACC would be anchored by Direct Primary Care physicians, nurse practitioners, and physicians’ assistants, serving as patient-centered medical homes. With smaller patient panels (about 750 patients per provider instead of 2000 to 2500 patients), Direct Primary Care Primary Care Providers (PCPs) could devote more time to each individual, fostering trust, improving continuity, and enhancing satisfaction. Preventive and coordinated care reduce downstream costs while strengthening doctor–patient relationships. Research suggests that reducing patient panels allows for more personalized care, improved patient outcomes, and greater physician satisfaction.
- Self-Regulation and Flexibility: Instead of one-size-fits-all federal medical treatment rules, each ACC defines its own clinical guidelines, benefit packages, and priorities. Cooperatives would provide optional home-birth services and alternative therapies as well as telemedicine, chronic care, and rural outreach. Local control fosters responsiveness and innovation.
4. Global Budgets: Operatingunder capitated global budgets, ACCs would receive a fixed per-memberamount to cover all health and social services. This eliminates incentives forunnecessary tests or procedures and drastically reduces bureaucratic overhead.Savings are reinvested into expanded services, lower premiums, and communitydevelopment initiatives. With a minimum number of “covered lives” in an ACCbeing at least 1,000,000 people, ACCs would be very likely to stay viablefinancially overtime.
- Transparent Competition: People choose their ACC based on services, health outcomes, member satisfaction, and cost. Transparency is central: ACCs publicly report expenditures, health outcomes, and member satisfaction to foster trust and informed choice.
- Participatory Governance: Decision-making resides with members, staff, an elected board, and a CEO, who collaboratively set priorities and allocate resources. This builds legitimacy and ensures that services reflect any community’s unique demographic and cultural profile.
- Doubling Provider Trainees: To support manageable caseloads, enrollment in U.S. medical schools must at least double. To provide primary care physicians, nurse practitioners, and physician assistants with manageable caseloads (750 patients per primary care provider (PCP) instead of 2000-2500 per PCP) and to account for the increased number of seniors with more healthcare needs, enrollment in US medical schools must at least double.
Funding and Financial Structure
ACCs would befinanced through a diversified mix:
- Risk-Adjusted Block Grants: from the US Department of Health and Human Services (e.g., Areas with higher need receive more funding.)
- Member Premiums, locally adjusted by age, income, and demographics.
- Community and Philanthropic Investment: for innovation, experimentation, and infrastructure.
Strategies tofree resources for patient care, social services, and lower member premiums oreliminate out of pocket costs include stopping:
- Excessive Administration: Accounting for at least 30% of total healthcare costs, including public and private insurance-related expenses and administrative burden on healthcare providers.
- Unnecessary or harmful medical interventions: See my book, Money Driven Medicine—Tests and Treatments That Don’t Work.
- Fraud: Estimated to range from 3% to 10% of total healthcare spending by the National Health Care Anti-Fraud Association.
ACCs address thefull continuum of need:
1. UniversalCoverage: Every US resident is enrolled in an ACC, closing all gaps.
2. MedicalCare: Preventive care(screenings, vaccinations), chronic disease management, dental care, and mentalhealth/addiction services.
3. Long-TermCare: Home-based andassisted-living support—services often excluded from Medicare and privateplans.
4. SocialServices: Housingassistance, food security, job training, and financial counseling.
5. AlternativeTherapies: E.g.,acupuncture, massage, prolotherapy, and midwife-assisted births. CostSavings: Capitated funding rewards prevention and efficiency.
6. ImprovedHealth Outcomes: Coordinated,community-based care reduces chronic disease by addressing root causes.
7. EmpoweredCommunities: Local healthcareand social services governance strengthen civic trust, participation, andresilience.
The ACCframework aligns with the Grand Bargains financial strategy: freeze total government health funding at the 2026 level through 2035 while expandinguniversal coverage and decentralizing delivery (approx.$6.3 trillion in 2026 and annually projected to 2035, a huge jump from $5.6trillion in 2025).
The most cited and realistic estimates project that the cost of healthcare in the U.S. will be around $9trillion in 2035, consuming approximately 20% to 22% of thecountry's total economic output (GDP).
Accountable Care Cooperatives represent a bold reimaginingof American healthcare—integrating universal access with fiscal responsibility.They advance the mission of the Grand Bargains project: rebuilding a societygrounded in solidarity, sustainability, and shared prosperity.
Pleaseforward this proposal to friends, family, and legislators. Questions orcomments? Email me at: grandbargainsbook@gmail.com
The Projected 10-Year Impact:
- $5 trillion saved on healthcare spending
- 23% reduction in the projected federal deficit
Five-Pronged Waste-Reduction Strategy
- Decentralize Regulation: Allow ACCs to develop their own clinical policies (e.g., choosing between bypass surgery or the Dr. Dean Ornish program for heart disease).
- Preserve Choice: Ensure patients and providers can choose their ACC.
- Mandate transparency—online disclosure of benefits, long-term care, and metabolic health programs (i.e., addressing obesity, type 2 diabetes, high blood pressure, and cardiovascular risks).
- Foster Competition: Compete on price, quality, and satisfaction.
- Freeze Spending: Cap government healthcare spending at 2026 levels through 2035.
Conclusion
Call to Action